
There will be some patients for which CPR would be inappropriate (final stages of terminal disease where CPR would not be successful). Neither patients nor relatives can demand treatment which is clinically inappropriate to them.
For patients with established DNAR orders going into procedures known to have a chance of causing cardiac/respiratory arrest (e.g. cardiac catheterisation, surgical operations), DNARs may be temporarily suspended on discussion with the patients.
Patients with capacity can refuse CPR in advance (as they can with all other treatments) without necessarily giving justification to their decisions. However the health team must ensure that their decision is not based on any inaccurate information or any misunderstanding.
If a person lacks capacity and has appointed a welfare attorney who has authority to make clinical decisions; (or via a court appointed guardian to act on the patient's behalf), they should be informed of the DNR. Any previously expressed wishes should be considered whilst making a DNR decision.
An example can be found here East Midland's DNR form
- Brain stem dead and maintained on a ventilator
- No blood borne viruses (hepatitis or HIV)
- No history of malignancy
- No systemic infections
BSD is diagnosed by 2 doctors (registered for at least 2 years, competent in their field, not members of the transplant team, at least 1 is a consultant) on two different occasions.
Legal time of death = when first test indicate BSD
Death is pronounced at the second set of tests
- Absent brain stem reflexes (pupillary, corneal, vestibulo-ocular, oculocephalic)
- Absent motor reflexes
- Apnoea with pCO2 > 6.65kPa (patient does not try to breath once ventilator has been disconnected)
The relatives views should be taken into grave consideration, and if they are opposed to the process then it may be wise to put their wishes first.
Authorization can be given only after it is clearly established that:
- The deceased has no objections to being used as an organ donor
- The relatives do not object
- There are no religious considerations
However payment does not include reasonable expenses (costs of removing, transporting, loss of earnings) paid to a living donor.
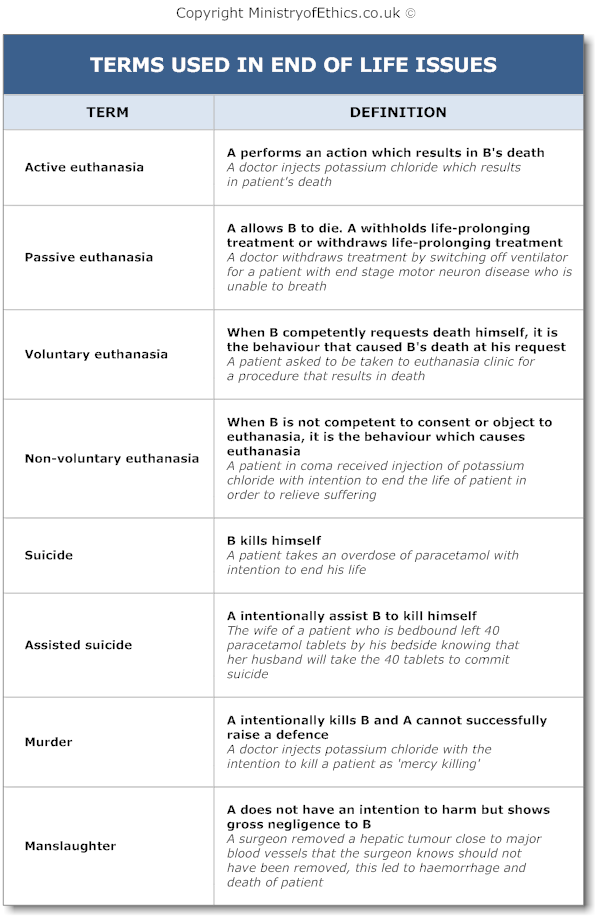
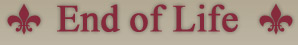
Key Legal Facts Regarding Euthanasia, Suicide and Assisted Suicide:
- Euthanasia is unlawful in England. In fact the law treats it as murder as "mercy killing" cannot be used as a defence.
- The law does not stop people from committing suicide, in fact the Suicide Act 1961 decriminalized suicide and attempted suicide. However, this does not extend to giving "claim right" to commit suicide (i.e. expect others to provide). As a result, this decriminalization should be interpreted as "liberty right", people cannot be stopped from committing suicide but one cannot demand a suicide.
- Assisted suicide in the forms of aid, abet, counsel or procure suicide is a criminal offence under the Suicide Act 1961.
- Although assisted suicide is unlawful, in reality "mercy killing" (treated as assisted suicide in law) is rarely prosecuted by the Crown Prosecution Service unless it is for public interest. Between 1982 to 1991, only 24 such cases were brought to court and 3 went to prison.
- The Director of Public Prosecutions produced a list of public factors that will be taken into account in a case of assisted suicide. Important factors in favour of prosecution are victim of age under 18, victim with mental illness or learning disability, victim does not have informed wish to commit suicide, victim did not have terminal illness and victim is able to commit suicide by himself.
Doctrine of double effect
The "Doctrine of double effect" which differentiates between the actions of the healthcare professional where death is either foreseen or intended. A healthcare professional who gives a large dose of morphine knows that the patient may die through respiratory depression but this is justifiable as it is intended for pain relief. Doctors in the UK, can prescribe unlimited amounts of pain relief so long as this is in the best interests of the patient, even if the patient's life is shortened as a result.
Contrast that with the injection of potassium chloride, where the only intention is to cause the death of the patient as there is no therapeutic value. This is legally murder.
Article 2 - the right to life [R(Pretty) v DPP]
Pretty argued that the right life extend to a right to control the manner of one's death and therefore a right to commit suicide. The House of Lords and European Court of Human Rights held that this article imposed a duty on the state to protect life, but not a right to die.
Article 3 - the right not to suffer torture or inhuman and degrading treatment
Pretty argued that not allowing her husband to perform assisted suicide is an inhuman treatment. The ECHR held that even if the condition that she is suffering is inhuman, it is not the result of treatment by the state or inflicted by the state.
Article 8 - the right to respect for private and family life
Interpretation of this article in R(Purdy) v DPP by the House of Lords led to the DPP to produce a list of public factors that will be taken into account in a case of assisted suicide as mentioned above.
Article 9 - The right to freedom of thought, conscience and religion
Pretty argued that she was being prevented from exercising her belief that it would be best if she ends her life. However, this was rejected on the basis that there was no interference with her believes. The state can prohibit actions motivated by a person's believes.
Opponents of euthanasia often use palliative care as the reason for opposing euthanasia. However, this viewpoint may compromise patient autonomy as patients are denied the choice of deciding how they should die.
The Doctrine of Double Effect distinguishes intention from foresight. Palliative care practitioners often used unlicensed high dose of analgesics to control symptoms. Administration of high dose analgesics with intention to relieve pain but may shorten the patient's life is considered lawful. However, it is not lawful if the administration of high dose analgesics has the intention to shorten the patient's life to relieve pain (i.e. euthanasia). This "doctrine" is subject to intense debate as many consider this as playing with words. However, this principle has been used in ruling of many high profile cases by Judges hence it is unlikely to be changed in any time soon.
Diagnosis of Death
The ethical and philosophical debates of the definition of death have troubled many great minds in history. What are the essential elements that constitute life? Does a person with a beating heart but has no awareness and response constitute life?
One would hope that on a pragmatic level the Law would provide a simpler answer. However the legal definition of death is surprisingly unclear. The current mainstream legal definition in England base on case law is brainstem death. It is clear from Re A that a patient who was on a ventilator and certified as brain stem dead was also legally dead, this conclusion was made according to expert medical opinion. It is also clear that persistent vegetative state (PVS) is not brainsteam dead and therefore patient is legally alive in Airedale NHS Trust v Bland [1993]. Expert medical opinion therefore has a great weight when judges consider the legal definition of death. Refer to the Department of Health's "A Code of Practice for the Diagnosis of Brain Stem Death" for practical steps in diagnosing brainstem death.
Legal Documents After Death
After the diagnosis of death, the most important legal document is the Medical Certificate of Cause of Death (MCCD), which is often known as "death certificate" used for any death occurring after the first 28 days of life. Any death of a live-born infant occurring within the first 28 days of life requires a different certificate known as the Neonatal Death Certificate. Any infant born with no signs of life after 24th week of pregnancy requires the Certificate of Still-birth. Refer to the "notes for doctors" for detailed guidance in the Medical Certificate of Cause of Death book.
The MCCD must not be confused with the process of cremation which is only applicable when the body is to be cremated. The application and process of cremation is governed by the Ministry of Justice Cremation Regulation 2008, refer to their Guidance for Doctors for detailed guidance in filling in the relevant forms. There is usually a payment to the doctors for filling in the cremation forms by the deceased family members, this practice has been challenged.
- A joint statement from the BMA, the Resuscitation Council (UK) and the Royal College of Nursing
- Cardiopulmonary resuscitation: Standards for clinical practise and training (RCAnaesthetists, RCP, ICS, the Resuscitation Council UK)
- http://www.uktransplant.org.uk Identification of potential donors of organs for transplantation: HSG (94)41 NHS Executive
- http://www.legislation.gov.uk/ukpga/1989/31/contents, Human Organ Transplants Act 2004


 . About
. About