
"Good mental health and resilience are fundamental to our physical health, our relationships, our education, our training, our work and to achieving our potential."
Mental health is an interesting and complicated aspect of medicine that has wide-reaching effects which are often unrealised or underestimated. The delicate topic of overriding refusal to treatment, even in those who are competent to make such a decision, necessitate added complexity in order to attempt to safeguard patients against those who may seek to abuse them.
Mental health acts attempt to address two different issues; the need to protect the patient him/herself and to protect the general public from the patient. It is evident that medical ethics has a large role to play in these situations as it is important to balance the four principles as suggested by Beauchamp and Childress (2001) of autonomy, beneficence, justice and non-maleficence. In this area of medicine where autonomy is often forcefully restricted it is important to consider these principles carefully in order to in order to reach a balanced decision.
There are five categories of mental disorders:
- Severe mental impairment (severe impairment of intelligence and social functioning)
- Mental impairment (impairment of intelligence and social functioning)
- Mental disorder (means mental illness)
- Psychopathic disorder (persistent disorder or disability of mind)
- Any other disorder or disability of mind
It does not include:
- Dependence on alcohol or drugs
- Sexual deviancy
- Promiscuity
NB. The 2007 amendment of the MHA 1983 has redefined a mental disorder and removed the latter two of the above exclusions, see below for further details.
Applications for compulsory detention can be made either by an approved mental health worker or by the nearest relative. For one to be compulsorily detained under the MHA, it is necessary to satisfy three conditions:
- The patient has a disorder of the mind
- The disorder is of sufficient severity to require treatment in hospital
- The health and/or safety of the patient, or the protection of the general public requires detention in hospital
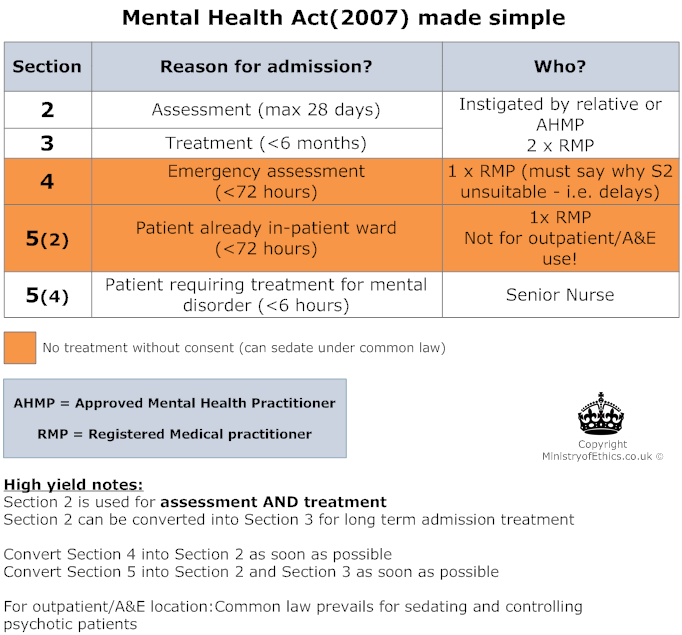
Most commonly used section
Can be applied for on the grounds that the patient:
- 'is suffering from mental disorder of a nature or degree which warrants the detention of the patient in a hospital for assessment (or for assessment followed by medical treatment) for at least a limited period' and that the patient
- 'ought to be so detained in the interests of his own health or safety or with a view to the protection of other persons'.
- Application requires the written recommendation of two registered medical practitioners, and is normally instigated by either the nearest relative or an Approved Social Worker (ASW), - note that this has been amended to Approved Medical Health Professional (AMHP) in the 2007 amendment, see below).
At least one of the medical practitioners should be approved by the Secretary of State as having special experience in the diagnosis or treatment of mental disorder.
- The length of time cannot exceed 28 days.
- It can be appealed (either by the patient or on behalf of him/her) within the first 14 days and will be heard by the Mental Health Review Tribunal.
- This may include treatment and assessment of the response to treatment.
This can be applied for on the grounds that the patient is:
- 'suffering from [mental disorder] of a nature or degree which makes it appropriate for him to receive medical treatment in a hospital'
- 'it is necessary for the health or safety of the patient or for the protection of other persons that he should receive such treatment and it cannot be provided unless he is detained'
- 'appropriate medical treatment is available'.
- Application requires the written recommendation of two registered medical practitioners, and is normally instigated by either the nearest relative or an approved social worker (ASW), - note that this has been amended to AMHP in the 2007 amendment, see below). At least one of the medical practitioners should be approved by the Secretary of State as having special experience in the diagnosis or treatment of mental disorder.
- It cannot be used to detain patients with 'any other disorder or disability of mind', unlike section 2.
- The length of time cannot exceed six months.
- It can be appealed (either by the patient or on behalf of him/her) within the first six months, during the second six months and then annually thereafter. It will be heard by the Mental Health Review Tribunal and a review is automatically instigated if no appeal has been requested within the first six months or within a 3-year period.
This can be applied for on one of the grounds stipulated in section 2.
- Application requires the written recommendation of one registered medical practitioner, and is normally instigated by either the nearest relative or an approved social worker (ASW - note that this has been amended to AMHP in the 2007 amendment, see below). The application must state the necessity of urgent admission and detainment under Section 2 AND why compliance of the usual provisions of Section 2 would 'involve undesirable delay'. It is desirable that the medical practitioner has had 'previous acquaintance with the patient'.
- The length of time cannot exceed 72 hours.
- A Section 2 is required if assessment beyond the 72 hours is required.
Section 4 and Section 5 does not allow treatment without consent (but under common law emergency treatment to contain the patient - i.e. sedation can be given in the best interests of the patient)
Section 5(2) can be applied for when a voluntary in-patient is no longer willing to stay in hospital and it is deemed necessary for him/her to stay. Cannot be used for outpatients or those attending A&E.
- Application requires the written recommendation of either the registered medical practitioner in charge of care (i.e. consultant) or a nominated deputy.
- The length of time cannot exceed 72 hours.
- A subsequent Section 2 or 3 is necessary if detainment beyond the 72 hours is required.
- Should detainment of a patient be required in a general hospital, compared to a psychiatric hospital, the consultant in charge of the patient's care would be required to fill out the necessary forms, or their nominated deputy. However, there is cross-over with common law here and it may be applicable to detain the patient under common law in order to prevent them from harming themselves.
This is similar to Section 5(2), except that the patient must already be receiving treatment for a mental disorder as an in-patient in a hospital.
This can be applied for under the grounds that the patient is:
- 'suffering from mental disorder to such a degree that it is necessary for his health or safety or for the protection of others for him to be immediately restrained from leaving the hospital' and
- 'it is not practicable to secure the immediate attendance of a practitioner [or clinician]'.
- Application requires the written recommendation of a 'nurse of the prescribed class' - i.e. a senior nurse.
- The length of time cannot exceed 6 hours.
- Psychosurgery requires both the consent of the patient and a second medical opinion
- Electroconvulsive therapy (ECT) requires a second medical opinion if consent is not obtained.
- Drug treatment for greater than three-months also requires a second medical opinion if consent is not obtained.
- Should treatment of a physical condition be deemed necessary, this could only be enforced using common law; i.e. in the patient's best interest. If, however, the physical condition does not require immediate attention, it preferable to increase the competency of the individual to consent (or refuse) treatment for the physical condition by treating the mental disorder first.
- Some argue that the MHA discriminates against mentally disordered people as it allows the detainment of those deemed to be a danger to the general public, even though other equally or more dangerous people who are not mentally disordered are not able to be detained due to infringement of civil liberties.
- MHA only applies to treatment of the mental disorder NOT the physical. However it can be used to treat physical disorders whereby the physical disorder is believed to contribute to the mental problem (i.e. enteral feeding of anorexics, whom doctors feel that hypoglycaemia is contributing to the incompetence)
- In the case of Re C (1993), a schizophrenic with gangrene in his foot refused to consent to an amputation and sought injunction to prevent it being done without his express consent. The court ruled that he could refuse consent despite suffering from delusions, as he was capable of understanding what was proposed and the consequences of his refusal.
- MHA allows doctors to provide treatment when patient is incompetent or refuses treatment for mental disorder
- Treatment must be reasonable for the condition
- Restrainment for treatment is allowed to allow for treatment to be carried out
- Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 5th ed. Oxford University Press; 2001.
- Mental Health Act 1983 [statute on the internet]. 1983 [cited 2011 Feb 1].
http://www.cqc.org.uk/_db/_documents/Mental_Health_Act_1983_201005272747.pdf - Mental Health Act 2007 [[statute on the internet]. 2007 [cited 2011 Feb 1].
http://www.legislation.gov.uk/ukpga/2007/12/contents


 . About
. About